The Florida Department of Health's Division of Children's Medical Services administers, with facilitation service from the National Institute for Children's Health Quality, a Statewide Network of Access and Quality program composed of five pediatric hematology-oncology organizations throughout Florida. Recognizing the importance of an adequate transition process to minimize morbidity and even mortality among youth with sickle cell disease (SCD), we have worked together for three years in several projects related to transition including educating medical providers and our own practices about SCD, transition, and GotTransition™ Six Core Elements ®. In June 2022, we began a new project with the aim statement that by December 2023, 80% or higher of the sickle cell patients ages 14-21 years attending clinic at the five hematology centers would have a readiness assessment and a transition plan updated at least once during the previous 12 months as assessed on monthly chart audits. At onset, 486 patients met criteria to be on a transition program due to age and cognitive ability. Two programs had previously participated in The Sickle Cell Trevor Thompson Transition Project (ST3P Up) (NCT 03593395), a Patient-Centered Outcomes Research Institute (PCORI) sponsored sickle cell transition study and learned to implement the GotTransition Six Core Elements. Three programs did not have transition programs implemented. The change ideas were either collective or implemented in a particular program depending on the program decision. The collective change ideas consisted of educating the clinical staff about GotTransition and quality improvement strategies, identifying eligible patients through patient roster, and implementing either monthly audits of ten random charts or reviewing charts of all patients who came the previous month for missed opportunities. The program-specific change ideas consisted of prospective review of patients who were scheduled to come to clinic within the week, staff huddles to discuss patients on transition, conversion of paper-based ASH or TIP-RFT sickle cell readiness assessment into electronic medical record (EMR) version, the use of smart phrases to document the readiness assessment and plan, and sharing ownership of the process with different members of the staff for sustainability. Data and learning from improvement strategies were reviewed twice a month with all group members in virtual one-hour meetings. Two quality improvement consultants encouraged and coached sites.
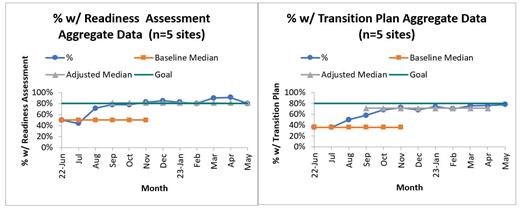
Figures show the run charts of the aggregate data. Per the Health Care Data Guide [Provost and Murray vbk://9781119690122] we used the median of the first three data points as a surrogate baseline in the absence of not having any prior data. We froze and extended the baseline median, looked at data collected after the changes were made and adjusted the median once improvement signals emerged. At the aggregate level, the mean percentage with a readiness assessment increased from 50% in June 2022 to 80% in May 2023 and the median performance throughout the 12 months increased from 50% to 81%. The mean percentage with a transition plan increased from 36% in June 2022 to 80% in May 2023 with an increase in the median performance across the 12 months from 36% to 78%. The activities which were identified as most successful were planning ahead of time to assess patients, having electronic document versions of the readiness assessments and documenting plans with smart phrases on the EMRs. Our network was successful in working together, sharing knowledge, and achieving goals. We plan to assess patient reported outcomes such as patient satisfaction with transition and completion of transition process as future projects.
Disclosures
Alvarez:Global Blood Therapeutics: Consultancy; Novartis: Consultancy.